[fusion_builder_container hundred_percent=”no” equal_height_columns=”no” menu_anchor=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” background_color=”” background_image=”” background_position=”center center” background_repeat=”no-repeat” fade=”no” background_parallax=”none” enable_mobile=”no” parallax_speed=”0.3″ video_mp4=”” video_webm=”” video_ogv=”” video_url=”” video_aspect_ratio=”16:9″ video_loop=”yes” video_mute=”yes” video_preview_image=”” border_size=”” border_color=”” border_style=”solid” margin_top=”” margin_bottom=”” padding_top=”” padding_right=”” padding_bottom=”” padding_left=”” admin_toggled=”no”][fusion_builder_row][fusion_builder_column type=”1_1″ layout=”1_1″ spacing=”” center_content=”no” hover_type=”none” link=”” min_height=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” background_color=”” background_image=”” background_position=”left top” background_repeat=”no-repeat” border_size=”0″ border_color=”” border_style=”solid” border_position=”all” padding=”” dimension_margin=”” animation_type=”” animation_direction=”left” animation_speed=”0.3″ animation_offset=”” last=”no”][fusion_text]
Best Practices for Blood Storage and Handling
[/fusion_text][/fusion_builder_column][fusion_builder_column type=”1_2″ layout=”1_2″ spacing=”” center_content=”no” hover_type=”none” link=”” min_height=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” background_color=”” background_image=”” background_position=”left top” background_repeat=”no-repeat” border_size=”0″ border_color=”” border_style=”solid” border_position=”all” padding=”” dimension_margin=”” animation_type=”” animation_direction=”left” animation_speed=”0.3″ animation_offset=”” last=”no”][fusion_text]
I am a Registered Nurse by training. I retired after 30 years in acute care hospitals, clinics, and public health. I worked directly with patients, in management, and served on committees. I also helped create policies and procedures.
[/fusion_text][fusion_text]
I say this to demonstrate that I am not an expert in blood components, but after researching the topic, there are some things I wish I had known when I worked in a surgical ICU years ago.
[/fusion_text][fusion_text]
I gave scores of blood components over the years. I was trained to “keep the units cold” until use, call the blood bank when I needed more or to have unused components picked up. I was told not to let the packed red cells get too warm, don’t administer them too cold, and don’t let them hang for more than four hours. We warmed cold blood next to our body or used warm water baths in old-fashioned blood warmers and used “blood pressure bags” to administer the blood quickly. We were to remind the Doctor when more than four units of RBC were given to help determine if coagulation might be an issue.
[/fusion_text][fusion_text]
All other protocols were based on proper identification of the ordered components and the patient. Is this the right patient and right blood? Did two licensed people cross check? I never remember recording component temperatures or time out of storage.
[/fusion_text][fusion_text]
While the majority of my online research indicated that highly technical studies are being done to provide answers to chemical and functional changes in blood once donated such as the effects of removing components, the age of the elements, etc., one thing is certain. Blood banks and any area that keeps blood components even for short periods of time need to have storage conditions and chain of custody temperature data available as a best practice in patient care.
[/fusion_text][fusion_text]
U.S. Medical workers administer about 14.7 million bags of blood to approximately five million patients each year to treat anemia or replace blood loss. NIH National Heart, Lung, and Blood Institute (NHLBI), www.nhlbi.nih.gov, 10-31-2017.
[/fusion_text][fusion_text]Standards are available for purchase from the AABB, formerly the American Association of Blood Banks at www.AABB.org.[/fusion_text][/fusion_builder_column][fusion_builder_column type=”1_2″ layout=”1_2″ spacing=”” center_content=”no” hover_type=”none” link=”” min_height=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” background_color=”” background_image=”” background_position=”left top” background_repeat=”no-repeat” border_size=”0″ border_color=”” border_style=”solid” border_position=”all” padding=”” dimension_margin=”” animation_type=”” animation_direction=”left” animation_speed=”0.3″ animation_offset=”” last=”no”][fusion_text]
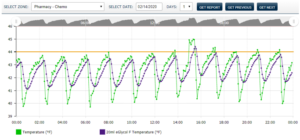
In essence, different blood components have different temperature storage needs.
- Platelets are stored at room temperature and must not be placed in any refrigerator.
- Refrigeration/storage units must be designed and operated for the explicit purpose of storing blood product.
- Blood products will only be issued for storage in these refrigerators when assurance is available they are working correctly and consistently.
- Handling of refrigerated components outside of main storage must be kept to a minimum to ensure that maximum temperature requirements are not exceeded.
– Red Cell components must not exceed 30 minutes at room temperature on each occasion
– Maintain blood components in a controlled temperature environment until administered
– Handle and store components in a way that minimizes the possibility of product tampering - Audible alarms that alert staff when temperatures are out of range are considered a best practice.
– Store red cells between 2C and 6C.
– Store Platelets between 20C and 24C.
– Fresh frozen plasma, cryo-depleted plasma, and cryoprecipitate are stored at or below -25C.
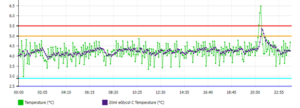
– Set Alarm trigger points within 0.5C of the storage temperature range.
[/fusion_text][fusion_text]
So for blood component logistics, what is the easiest way to control that which is controllable?
First, I would make sure I have the infrastructure in place to manage my blood supply including:
- Obtaining the cold chain record of any component I am receiving. This should including copies of all necessary records.
- Having the required purpose-built storage units available.
- Ensuring the temperature recording devices are certified and calibrated, and the certificates and temperature records are readily available.
- Having transport protocols in place that maintain and verify the accuracy of the cold chain by using temperature data logging devices that can record the time the components are in transport and will alarm qualified personnel of any problems before wastage can occur.
Second, thoroughly train staff on blood storage and transportation requirements for my institution.
Third, work with a knowledgeable and competent vendor to ensure safety for the patients, the staff, and the institution.
[/fusion_text][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]